The Truth About Complete Androgen Insensitivity Syndrome (CAIS) - What does science has to say about it?
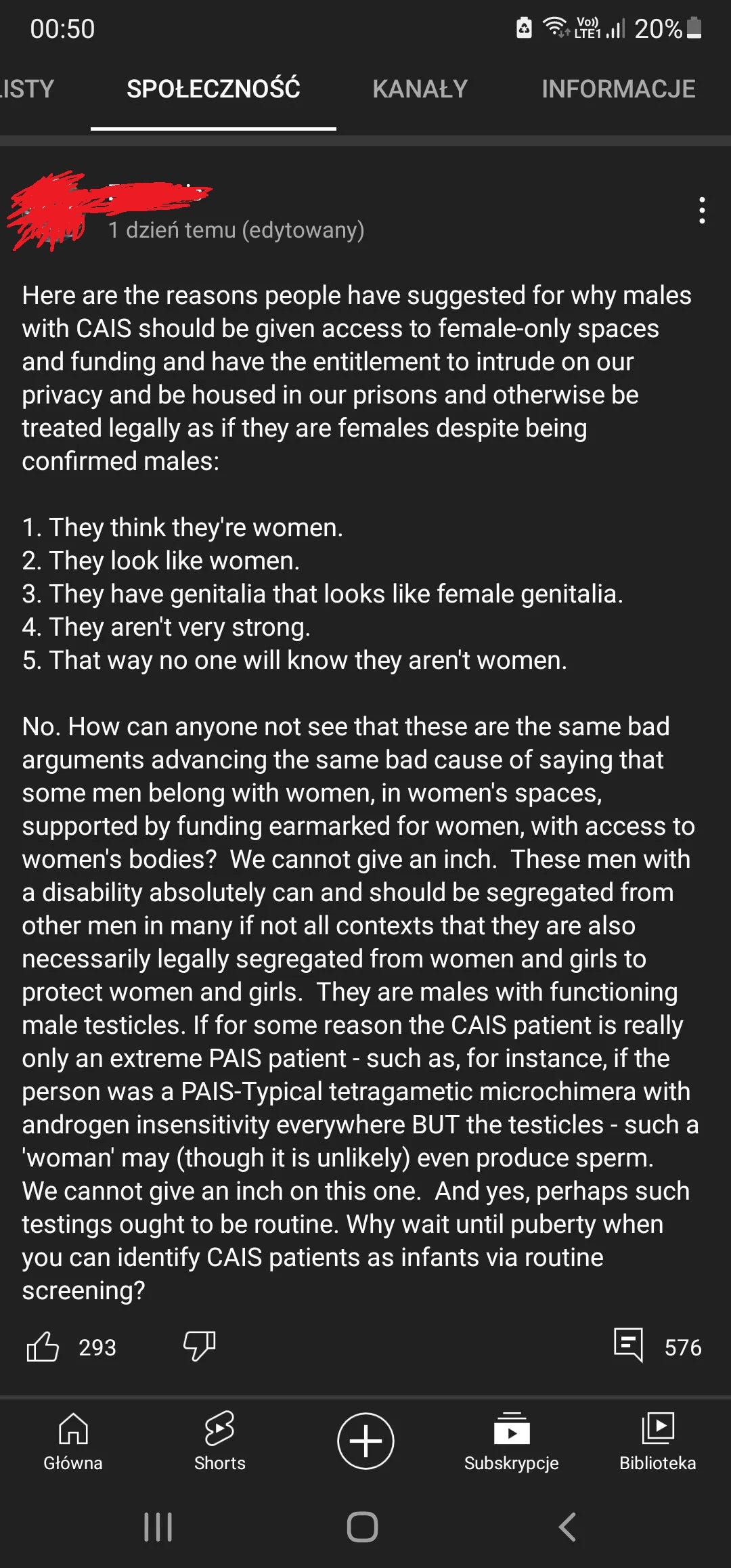
There are those GC who believe that this atypical female development should be regarded as imposters and imprisoned in men's prisons thrown out of women's spaces.
Complete Androgen Insensitivity Syndrome (CAIS) is a unique condition that affects sexual development. Individuals diagnosed with CAIS have a 46 XY chromosomal pattern typically associated with males, but their physical traits or phenotype and genetic expression or genotype are female. This means that, despite having a genetic make-up linked with male development, they physical bodies are female. This transformation begins as early as six weeks into pregnancy, with estrogen, a female hormone, activating genes in the fetus to develop female physical characteristics.
The cause of this unique condition lies in the underdeveloped male reproductive organs, known as gonads or testes, present inside the body. These gonads perform the hormonal role typically carried out by ovaries, producing estrogen that further promotes female development. However, these individuals lack a uterus and ovaries, a discrepancy that arises due to their cells' resistance to testosterone, a male hormone. This resistance prevents testosterone from triggering the development of male physical characteristics, thus leading to the formation of a female body with partially developed male reproductive organs.
Androgen Insensitivity Syndrome (AIS) has two subtypes: Complete Androgen Insensitivity Syndrome (CAIS) and Partial Androgen Insensitivity Syndrome (PAIS). Both are distinct conditions and should not be confused with each other.
Understanding the development of CAIS involves getting to grips with the role of androgens. Androgens are hormones critical for reproductive health and physical development, the most well-known of which is testosterone, produced in the male testes. Other androgens produced by our bodies include androstenedione, dehydroepiandrosterone (DHEA), DHEA sulfate (DHEA-S), and Dihydrotestosterone (DHT). DHEAS, DHEA, and androstenedione all serve as precursors to testosterone.
The Androgen Receptor (AR) gene plays a crucial role in AIS. It codes for the androgen receptor protein, which is present in numerous body tissues. This protein binds to androgens, forming a complex that regulates the activity of genes responsive to androgens. While the AR's primary function is to govern male sexual development, it also has roles in both males and females, such as regulating hair growth, sebaceous and apocrine gland activation, and libido.
In AIS patients, over 600 different AR gene mutations have been discovered. These mutations are alterations in the DNA sequence that can impact one or more base pairs. Some mutations cause defects in the AR protein, while others result in abnormal receptors that cannot bind to androgens. In such cases, cells are unable to utilize androgens. In CAIS, a genetic mutation fully eliminates the function of the androgen receptor, causing the developing fetus to rely solely on estrogen. This results in women with CAIS having minimal body hair and no body odor due to their resistance to androgens.
Most AR mutations originate in germ cells, cells involved in reproduction. Approximately two-thirds are inherited from mothers carrying an altered copy of the AR gene on their X chromosome. Other mutations can occur in the mother's egg cells before conception or during fetal development. Some may even arise in somatic cells (non-reproductive cells), and hence are not inherited.
Detecting CAIS can be challenging. Often, the condition is discovered during puberty when menstruation does not begin. Individuals with CAIS have a typically female appearance and internal underdeveloped male gonads incapable of fertilization or sperm production. They also psychologically identify as female. Absence of internal female reproductive organs occurs due to the testes' Sertoli cells, which produce a hormone called anti-Müllerian hormone. This hormone prompts the regression of Müllerian structures (uterus, cervix, and deeper part of the vagina).
Well-being
CAIS produces a lot of distress, so psychological support is essential. Healthcare specialists and psychologists can help them understand their bodies and sex development. Health issues are substantially less significant in comparison with other DSDs such as Klinefelter syndrome. However, there is an issue with suicidal thoughts and despair and mental suffering. The discovery that these women can never have children or become pregnant, as well as the persistent superstition around gonads as a determinant of “maleness,” remains to this day, and are maintained even by feminists (see the Twitter clips).
Sex life Women with CAIS can have a normal sex life. However, they often report sexual difficulties associated with vaginal hypoplasia (when the vagina is not wholly developed)
Immune and metabolic issues Some studies show CAIS may be associated with increased susceptibility to infections and autoimmune diseases. They may also be more likely to develop metabolic syndrome, diabetes, and heart conditions.
References
1- Tyutyusheva, Nina, et al. "Complete androgen insensitivity syndrome: from bench to
bed." International journal of molecular sciences 22.3 (2021): 1264.
2- Overview Androgen Insensitivity Syndrome, 2021. NHS. Available at:
https://www.nhs.uk/conditions/androgen-insensitivity-syndrome/. Access:
01/26/2022.
3- AR gene, 2020. Medline Plus. Available at:
https://medlineplus.gov/genetics/gene/ar/#conditions. Access: 01/26/2022.
4- Androgen insensitivity syndrome, 2020. Medline Plus. Available at:
https://medlineplus.gov/genetics/condition/androgen-insensitivity-syndrome/.
5- Gulía C, Baldassarra S, Zangari A, Briganti V, Gigli S, Gaffi M, Signore F, Vallone C,
Nucciotti R, Costantini FM, Pizzuti A, Bernardo S, Porrello A, Piergentili R. Androgen
insensitivity syndrome. Eur Rev Med Pharmacol Sci. 2018 Jun;22(12):3873-3887. doi:
10.26355/eurrev_201806_15272. PMID: 29949163.
6- Minto CL, Liao KL, Conway GS, Creighton SM. Sexual function in women with
complete androgen insensitivity syndrome. Fertil Steril. 2003 Jul;80(1):157-64. doi:
10.1016/s0015-0282(03)00501-6. PMID: 12849818.
7- Czech, D.P., Lee, J., Sim, H., Parish, C.L., Vilain, E. and Harley, V.R. (2012), The human
testis-determining factor SRY localizes in midbrain dopamine neurons and regulates
multiple components of catecholamine synthesis and metabolism. Journal of
Neurochemistry, 122: 260-271. https://doi.org/10.1111/j.1471-4159.2012.07782.x
8- Tahira, AC, Barbosa, AR, Feltrin, AS, et al. Putative contributions of the sex
chromosome proteins SOX3 and SRY to neurodevelopmental disorders. Am J Med
Genet Part B. 2019; 180B: 390– 414. https://doi.org/10.1002/ajmg.b.32704
9- Androgens, 2021. Cleveland Clinic. Available:
https://my.clevelandclinic.org/health/articles/22002-androgens. Access: 01/27/2022.
10- Heo YJ, Ko JM, Lee YA, et al. Two Korean girls with complete androgen insensitivity
syndrome diagnosed in infancy. Ann Pediatr Endocrinol Metab. 2018;23(4):220-225.
doi:10.6065/apem.2018.23.4.220
11- Valeri, C., Lovaisa, M. M., Racine, C., Edelsztein, N. Y., Riggio, M., Giulianelli, S.,
Venara, M., Bedecarrás, P., Ballerini, M. G., di Clemente, N., Lamb, C. A., Schteingart, H.
F., & Rey, R. A. (2020). Molecular mechanisms underlying AMH elevation in
hyperoestrogenic states in males. Scientific reports, 10(1), 15062.
https://doi.org/10.1038/s41598-020-71675-7

This is a bit tricky to read. The formatting has gone skew-whiff. It is a bit of a nuisance on Substack but hyperlinks do not turn into links automatically, you have to add them manually using the "link button" and inserting the URL.